Chapter 2: The Science of Depression
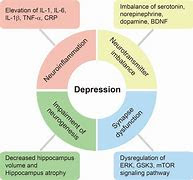
Depression is often described as a disorder of
the mind, but its roots run much deeper, intertwining with the intricate
workings of the brain and body. To truly understand depression, we must explore
the science behind it—how it alters brain chemistry, how genetics and biology
play a role, and how external factors like stress and trauma can trigger or
exacerbate the condition. This chapter delves into the fascinating and complex
science of depression, shedding light on the biological and physiological
mechanisms that underpin this mental health disorder.
The
Brain and Depression: Neurotransmitters, Hormones, and Brain Chemistry
At the heart of depression lies the brain, an
organ so complex that scientists are still unraveling its mysteries. Depression
is not simply a "mood disorder"; it is a condition that involves
significant changes in brain structure, function, and chemistry. Let’s explore
the key players in the brain that contribute to depression.
Neurotransmitters:
The Brain’s Chemical Messengers
Neurotransmitters are chemicals in the brain
that facilitate communication between nerve cells (neurons). They play a
crucial role in regulating mood, emotions, and behavior. Three
neurotransmitters are particularly important in understanding depression:
1. **Serotonin:** Often referred to as the "feel-good"
neurotransmitter, serotonin helps regulate mood, sleep, appetite, and
digestion. Low levels of serotonin are strongly associated with depression.
Many antidepressant medications, such as selective serotonin reuptake
inhibitors (SSRIs), work by increasing serotonin levels in the brain.
2. **Dopamine:** Known as the "reward" neurotransmitter, dopamine
is involved in motivation, pleasure, and the brain’s reward system. Reduced
dopamine activity can lead to feelings of apathy, lack of motivation, and
anhedonia (the inability to feel pleasure), all of which are common symptoms of
depression.
3. **Norepinephrine:** This neurotransmitter is linked to alertness, energy,
and the body’s stress response. Low levels of norepinephrine can contribute to
fatigue, lack of focus, and a general sense of lethargy, which are often seen
in depression.
The imbalance of these neurotransmitters
disrupts the brain’s ability to regulate mood and emotions, creating the
conditions for depression to take hold.
**The Role of
Brain Structures**
Depression is
also associated with changes in specific brain regions:
The
Prefrontal Cortex:
This area of the brain is responsible for
decision-making, problem-solving, and regulating emotions. In people with
depression, the prefrontal cortex often shows reduced activity, which can lead
to difficulties in concentration, decision-making, and emotional regulation.
- **The Hippocampus:** The hippocampus plays a key role in memory and
learning. Chronic stress and depression can cause this region to shrink,
impairing memory and contributing to feelings of hopelessness.
- **The Amygdala:** The amygdala is involved in processing emotions,
particularly fear and stress. In depression, the amygdala may become
overactive, leading to heightened feelings of anxiety and sadness.
The
HPA Axis and Hormones
The hypothalamic-pituitary-adrenal (HPA) axis
is a complex system that regulates the body’s response to stress. When the HPA
axis is dysregulated, it can lead to an overproduction of cortisol, the body’s
primary stress hormone. Elevated cortisol levels have been linked to
depression, as they can disrupt sleep, impair cognitive function, and
contribute to feelings of fatigue and irritability.
**Genetic
and Biological Factors**
While environmental factors play a significant
role in depression, genetics also contribute to an individual’s susceptibility
to the condition. Research has shown that depression can run in families,
suggesting a hereditary component.
The
Role of Genetics**
Studies of twins and families have found that
depression has a heritability rate of approximately 30-40%. This means that
genetics account for about one-third of the risk of developing depression.
Researchers have identified several genes that may be associated with
depression, many of which are involved in regulating neurotransmitters like
serotonin and dopamine.
However, having a genetic predisposition does
not guarantee that someone will develop depression. Environmental factors, such
as trauma or chronic stress, often interact with genetic vulnerabilities to
trigger the condition.
Epigenetics is the study of how environmental
factors can influence gene expression without altering the underlying DNA
sequence. Stress, trauma, and other environmental factors can cause epigenetic
changes that increase the risk of depression. For example, chronic stress may
lead to changes in the expression of genes involved in the HPA axis, making
individuals more susceptible to depression.
The
Role of Stress and Trauma in Triggering Depression
Stress and trauma are among the most
significant environmental factors that can trigger or exacerbate depression.
Let’s explore how these factors impact the brain and contribute to the
development of depression.
**Acute
vs. Chronic Stress**
Stress is a natural response to challenging
situations, but when it becomes chronic, it can take a toll on both the brain
and body. Acute stress, such as preparing for an exam or giving a presentation,
is short-term and can even be beneficial in small doses. Chronic stress, on the
other hand, is long-lasting and can lead to significant changes in brain
structure and function.
Chronic
stress can
- Reduce the size of the hippocampus, impairing memory and learning.
- Increase the size and activity of the amygdala, leading to heightened
anxiety and emotional reactivity.
- Disrupt the balance of neurotransmitters, contributing to mood disorders
like depression.
Trauma
and Depression
Trauma, particularly during childhood, is a
major risk factor for depression. Adverse childhood experiences (ACEs), such as
abuse, neglect, or the loss of a parent, can have long-lasting effects on
mental health. Trauma can alter the brain’s stress response system, making
individuals more vulnerable to depression later in life.
Post-traumatic stress disorder (PTSD) is
closely linked to depression, as both conditions involve deregulation of the
HPA axis and changes in brain structures like the hippocampus and amygdala.
**How
Depression Affects the Body: Physical Symptoms and Health Risks**
Depression is not just a mental health
condition; it has profound effects on the body as well. The mind and body are
deeply interconnected, and the physical symptoms of depression can be just as
debilitating as the emotional ones.
Physical
Symptoms of Depression
- **Fatigue:** Persistent feelings of exhaustion are one of the most common
physical symptoms of depression. This fatigue is not relieved by rest and can
make even simple tasks feel overwhelming
- **Sleep Disturbances:** Depression often disrupts sleep patterns, leading
to insomnia (difficulty falling or staying asleep) or hypersomnia (excessive
sleeping).
- **Appetite Changes:** Depression can cause significant changes in
appetite, leading to weight loss or gain. Some people may lose interest in
food, while others may turn to food for comfort.
- **Chronic Pain:** Depression is frequently associated with unexplained
aches and pains, such as headaches, back pain, or muscle soreness. This is
because depression can lower the pain threshold, making individuals more
sensitive to physical discomfort.
- **Digestive Issues:** Depression can affect the gut-brain axis, leading to
symptoms like nausea, diarrhea, or constipation.
Health
Risks Associated with Depression
Depression is not just a mental health issue;
it is a risk factor for a range of physical health problems. These include:
- **Cardiovascular Disease:** Depression is linked to an increased risk of
heart disease and stroke. This may be due to the effects of chronic stress and
inflammation on the cardiovascular system.
- **Diabetes:** Depression can contribute to the development of type 2
diabetes by affecting insulin sensitivity and promoting unhealthy lifestyle
behaviors.
- **Immune System Dysfunction:** Depression can weaken the immune system,
making individuals more susceptible to infections and illnesses.
- **Chronic Inflammation:** Depression is associated with elevated levels of
inflammatory markers in the body, which can contribute to a range of health
problems, including autoimmune disorders and cancer.
**Conclusion**
The science
of depression reveals a complex interplay between the brain, body, and
environment. From imbalances in neurotransmitters and changes in brain
structures to the impact of genetics, stress, and trauma, depression is a
multifaceted condition that affects every aspect of a person’s life. By
understanding the biological and physiological mechanisms behind depression, we
can better appreciate the challenges faced by those living with this condition
and work toward more effective treatments and interventions.
In the next
chapter, we will explore the different types of depression, from major
depressive disorder to seasonal affective disorder, and examine how these
variations manifest in individuals. Understanding the diversity of depressive
disorders is essential for providing personalized care and support.
https://sites.google.com/view/love-is1/home




No comments:
Post a Comment